The United States Department of Health and Human Services has several sub-agencies that handle specific tasks. One of those agencies is the Centers for Medicare and Medicaid Services (CMS), which is responsible for managing and administering federal healthcare programs, including Medicare and Medicaid. CMS also works to prevent fraud in health care, ensure safe nursing home practices, and advocate for modern healthcare reform.
4 Programs Managed by CMS
- Medicare
- Medicaid
- Children’s Health Insurance Program (CHIP)
- Health Insurance Marketplace (Affordable Care Act)
Several programs make up the nation’s healthcare system to ensure that each American has access to the medical insurance they need for quality care. The United States Department of Health and Human Services is the primary federal agency tasked with overseeing each federal health insurance program. However, the CMS ultimately takes charge of the fine details.
Medical care for the elderly, children, families, and individuals is available through the Centers for Medicare and Medicaid Services. Some of the included programs cover many medical services for free, while others have low-cost premiums for easy access to care.
What Is CMS?
The Centers for Medicare and Medicaid Services is a branch of the Department of Health and Human Services (HHS) that oversees, manages, and administers federal health insurance programs. In addition to Medicare and Medicaid, CMS also manages the Children’s Health Insurance Program (CHIP) and the Health Insurance Marketplace through the Affordable Care Act.
Each CMS health insurance program is a government-backed program. The U.S. government and tax dollars fund the income-based programs. Only U.S. citizens who meet eligibility guidelines based on their incomes, household composition, and other factors can receive coverage through a plan.
The primary goal of CMS is to provide Americans with a basic health program that covers health care necessities, such as primary care, prescriptions, and lab tests. Children, families, individuals, and elderly citizens may all qualify for specific programs.
The CMS also controls other aspects of healthcare for American citizens, like simplifying healthcare administration, ensuring that long-term care facilities meet certain standards, and implementing Affordable Care Act laws.
Additionally, CMS works with healthcare providers and insurance companies to reduce and prevent insurance fraud. Healthcare research and forecasting also help CMS make important healthcare decisions that can affect quality standards and healthcare costs.
History of CMS
Although not officially founded until 2001 as the Centers for Medicare and Medicaid Services, the basis for CMS dates back to the 1960s, when the Medicaid and Medicare programs were formed. The programs began under Lyndon B. Johnson’s presidency as part of the Social Security Act Amendments.
With the passing of the programs into law, Johnson pushed forward legislation that had dwindled for about 20 years and stalled the ability for elderly Americans to have affordable, quality healthcare.
In 1977, the U.S. government took another step forward with the establishment of the Health Care Finance Administration (HCFA) to manage the nation’s Medicare and Medicaid programs. In 2001, the HCFA changed its name to the Centers for Medicare and Medicaid Services, although the program continued to oversee these programs. The CMS later added CHIP and the Health Insurance Marketplace to its repertoire of programs.
4 Programs Managed by CMS
The four programs managed by the Centers for Medicare and Medicaid Services are Medicare, Medicaid, CHIP, and the Healthcare Marketplace. Learn more about each program and its eligibility, costs, and coverage.
1. Medicare
Medicare is health insurance for people 65 and older and some younger people with disabilities. The health care program is designed to help seniors and other eligible individuals afford quality health care, including hospital stays, primary care, preventative services, and medical equipment.
Eligibility
To qualify for Medicare coverage, a person must be 65 or older, have an eligible disability, or have end-stage renal disease. People younger than 65 can qualify if they’ve received Social Security benefits for at least 24 months. Senior recipients must have worked for 10 years at jobs paying Medicare tax to receive benefits.
What It Covers
Medicare comes in different parts (A, B, C, and D), which we’ve described in detail below. Recipients can choose which coverage they’d like to have based on their medical needs. Overall, the Medicare program can cover hospital visits and stays, emergency care, outpatient visits, and prescription drug coverage.
Medicare Part A
Medicare Part A covers inpatient hospital care, care in a skilled nursing facility, hospice care, and home health care. This coverage is best for individuals who require long-term medical care for an ongoing condition. However, Medicare generally only pays for a specific amount of time, such as 100 days in a skilled nursing facility per benefit period and up to 100 days of continuous home health care.
Medicare Part B
Part B Medicare coverage is for primary and outpatient care. Individuals can use this coverage for regular doctor visits, visits to specialists, therapy services, lab tests, ambulance services, and durable medical equipment.
Medicare Part C
Medicare Part C is also called Medicare Advantage. A Medicare Advantage plan goes through a private health insurance company but follows Medicare rules. Eligible individuals may choose to go this route if they can receive certain benefits through the health insurance company that they may not receive going through a regular Medicare plan.
Medicare Part D
Medicare Part D pays for prescription drugs. Some drugs are covered under Medicare Part B, but Part D offers the most widespread coverage. Part D is available through a regular Medicare plan or Medicare Advantage plan.
Costs
Medicare beneficiaries pay different costs based on their Medicare program and income. Most people do not pay a premium for Medicare Part A, but they could have deductibles and coinsurances for services. Part B premiums are based on beneficiaries’ income. Part C and D premiums vary based on the plans beneficiaries choose.
How to Apply
You can start the process to apply for original Medicare or a Medicare Advantage plan on the Medicare.gov website. People who have applied for Social Security disability benefits may already have an application for Medicare on file.
2. Medicaid
Medicaid can benefit people who may not qualify for Medicare, although some individuals are beneficiaries of both programs. Medicaid is specifically for low-income individuals and families and other vulnerable populations, such as pregnant women, people with disabilities, and children.
States can choose how to operate their Medicaid programs to an extent. For instance, states can set income guidelines, cost-sharing requirements, and work requirements for people to qualify for Medicaid.
Eligibility
Generally, individuals applying for Medicaid must be residents of the state in which they apply and meet income guidelines. The specific requirements may vary by state. Some states have a medically needy program to allow some individuals to become eligible for Medicaid if their income is too high to meet regular guidelines.
What It Covers
What does Medicaid cover? Medicaid typically covers most health care services, such as hospital stays, outpatient care, prescription drugs, and medical equipment. However, states can determine the full range of benefits for Medicaid recipients. Vision and dental services are examples of optional coverages that states may choose to include.
Costs
Many Medicaid recipients have no monthly premiums for Medicaid, but some states do charge low-cost premiums, deductibles, copays, or coinsurance. Some recipients may also need to participate in cost-sharing if they have higher incomes.
How to Apply
Apply for Medicaid on the Medicaid.gov website, by calling the Medicaid hotline, or by visiting your local jobs and family services office.
3. Children’s Health Insurance Program (CHIP)

The Children’s Health Insurance Program (CHIP) is a health insurance program with benefits for children and, in some states, pregnant women. This program works through Medicaid, so it operates similarly, allowing states to choose their specific eligibility guidelines and coverage offerings.
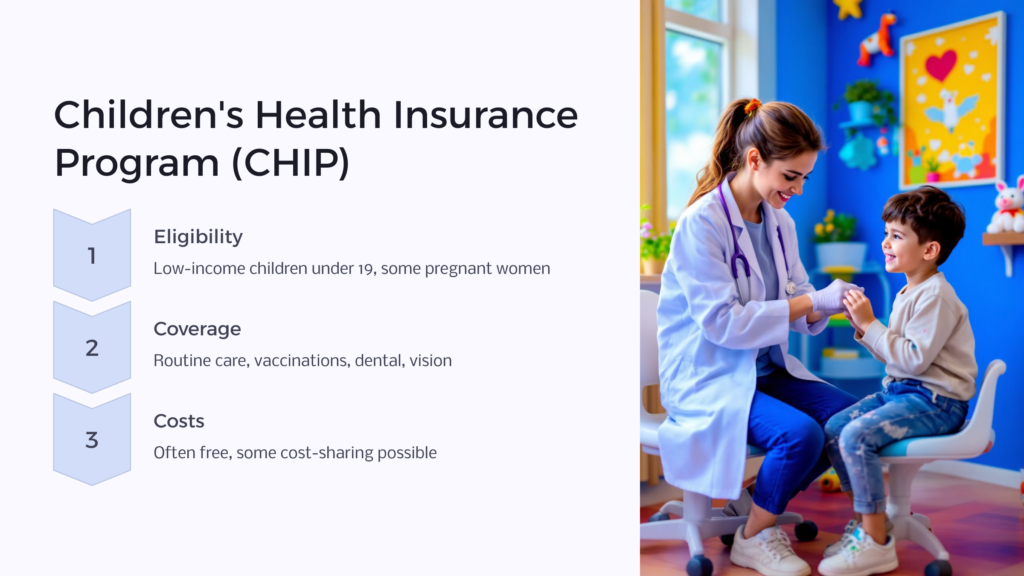
Eligibility
Each state can outline its specific eligibility guidelines. However, recipients must qualify based on their income, household status, and demographics. This program is designed for low-income children and pregnant women. To qualify, children must be under 19 years of age and ineligible for Medicaid or a private health insurance plan. Pregnant women meeting income guidelines may qualify in their state.
What It Covers
Much like Medicaid, CHIP covers most routine and specialist care services. Most states also cover a wide range of diagnostic, treatment, and prevention services. Vaccinations, dental coverage, vision coverage, and well-child visits may also be included, depending on your state.
Costs
For many recipients, CHIP has free monthly premiums. However, you may still be responsible for paying some expenses, like copays or coinsurance. Check with your state to see if it participates in cost-sharing for CHIP.
How to Apply
You can apply for CHIP via your state’s Medicaid or health care website or by visiting a local Medicaid center for an application or assistance with applying.
4. Health Insurance Marketplace (Affordable Care Act)
Signed into law in 2010, the Affordable Care Act sought healthcare reform. The law encouraged uninsured Americans to get healthcare. Lower-income Americans could receive health insurance through the Health Insurance Marketplace with discounted monthly premiums.
Eligibility
To qualify for Marketplace coverage, you must be a United States citizen, not be incarcerated, and meet income guidelines. You can fill out a few screener questions on the Healthcare Marketplace (Healthcare.gov) website to determine if you could be eligible for a plan.
What It Covers
Health Insurance Marketplace plans come from health insurance companies within your state. Each company determines specific plan benefits, including what type of services are fully covered and which ones require co-pays.
However, every Marketplace plan must cover mandatory services set by the ACA, including pregnancy and childbirth services and prescription drugs. Dental and vision plans are separate, but you can purchase them through the Marketplace.
Costs
Your cost for healthcare through the Marketplace depends on your income and the plan you choose. The Marketplace offers Bronze, Silver, Gold, and Platinum tiers, with the latter offering the best coverage but higher premiums. Estimate your costs on the Marketplace website.
How to Apply
Apply for coverage by filling out an application on Healthcare.gov. If eligible, the Marketplace will show you your qualifying plans to compare and choose from.
Programs of the Centers for Medicare and Medicaid Services (CMS)
The Centers for Medicare and Medicaid Services manage programs that are extremely beneficial to the groups who need them. Medicare is one such program with notable perks for elderly citizens, including affordable access to care and coverage for durable medical equipment.
However, Medicare premiums continue to increase, making it somewhat challenging for limited-income seniors to afford their medical care. Some coinsurance and deductibles for Medicare Part A plans are also on the rise.
Still, CMS continues to fight and advocate for those needing federal healthcare, including Medicare recipients. Recently, for instance, CMS has proposed a rule to lower out-of-pocket prescription costs for Medicare Part D recipients. Additionally, the No Surprises Act was implemented in 2022 to protect insured patients from surprise medical bills from out-of-network providers.
For more information about the CMS, its programs, and how to apply for a government health insurance plan, visit the CMS.gov website. You can also visit or call your local Department of Health and Human Services to learn about each program, its eligibility guidelines, and its application process.
 Benefits.com Advisors
Benefits.com Advisors
With expertise spanning local, state, and federal benefit programs, our team is dedicated to guiding individuals towards the perfect program tailored to their unique circumstances.
Rise to the top with Peak Benefits!
Join our Peak Benefits Newsletter for the latest news, resources, and offers on all things government benefits.